Prototyping Participation
3D Printing Co-Design into Healthcare
In 2016, while working at the Design for Health & Wellbeing Lab, I completed a Masters in Industrial Design at AUT University with a project focused on exploring the intersection between co-design and 3D printing within a healthcare environment. Due to a 3-year long embargo (restricted access), I wasn’t able to share my thesis until now (2020).
Written below is a brief overview of the research, as well as some of the images from different concepts that were created during the course of the project. If you’re interested in viewing the full thesis, you can download it as a PDF by the link below.
Research Question
How can 3D printing be used as a design tool to help facilitate co-design in healthcare?
Summary
Increasingly accessible, affordable and technically viable, 3D printing is now being used for a number of high-end healthcare applications, including orthopaedic implants, prosthetics and dentistry casting. However, these applications are often driven by industries that aren’t embedding themselves within the complex environments for which they are designing. Without this embedded approach, these groups potentially lack an accurate, in-depth understanding of the people they’re designing for.
In contrast, my practice-based research operated within a hospital environment and alongside healthcare professionals who possessed a practical understanding of relevant clinical requirements and patient experiences. Using a co-design methodology, a series of problems were identified and developed in regular workshop-style interactions.
As a way to help facilitate these interactions, objects were designed and printed that not only leveraged the specific properties of 3D printing – rapid, iterative, and customisable – but also worked as a tool for co-design. These tangible 'probes' were not a forerunner of the future product, but rather vehicles for observation, reflection, interpretation, discussion and expression. Chosen objects helped to create a bridge between the worlds of design and health, acting as a common language between the designer and the participant in order to help establish a shared understanding. In turn, this shared understanding provided a stronger foundation for the collaborative identification and development of design opportunities, suitably linking a specific clinical problem with the capabilities of technology.
In this way, 3D-printed probes enabled my co-design interactions to evolve from passive exchanges of knowledge to more effective, active relationships. These relationships may be the key to unlocking a more reliable model for design outcomes in results- driven environments such as hospitals.
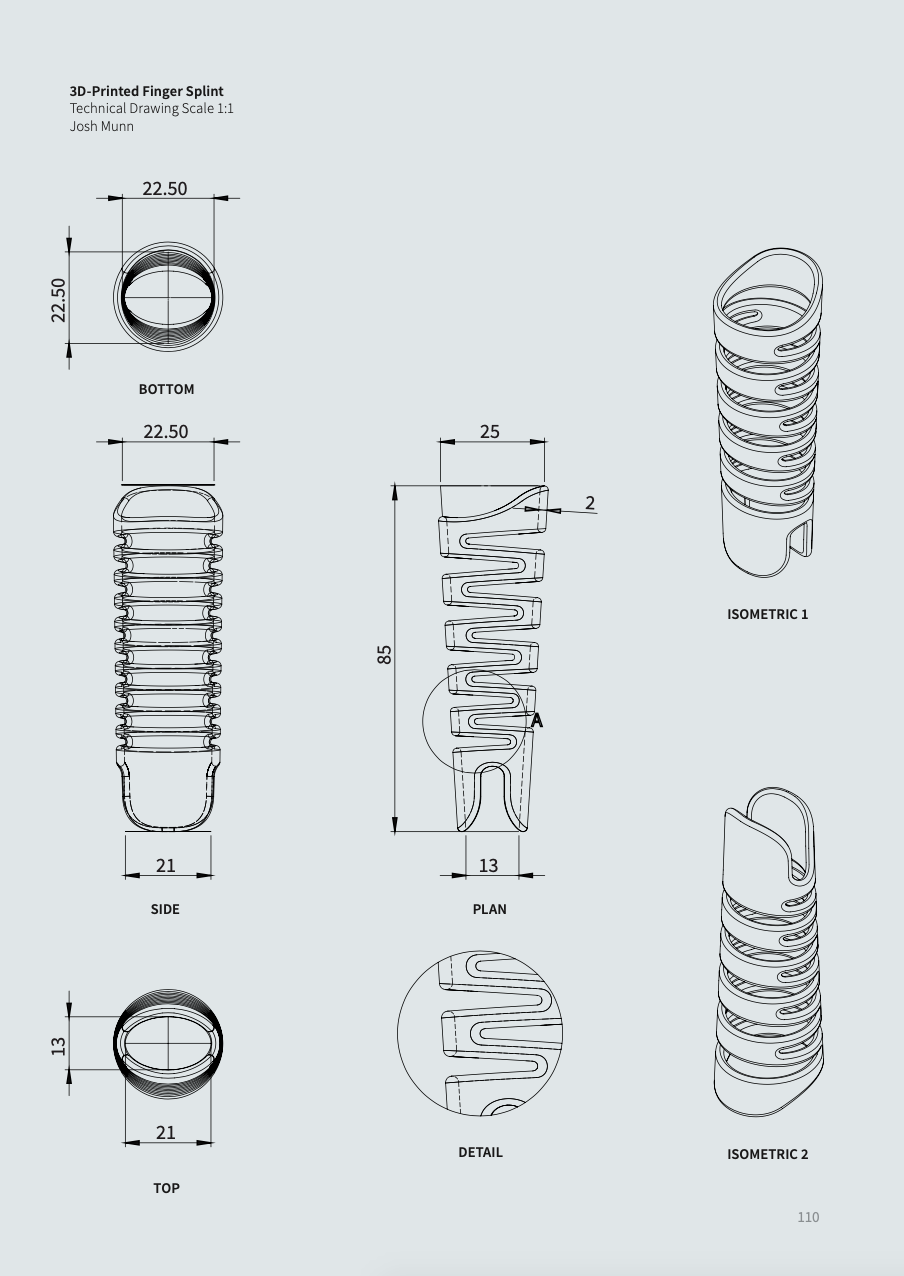
Finger Splint Concept
Problem
3D-printed finger splints were suggested by a plastic surgeon based on his reservations around the accuracy and effectiveness of traditional splint- making techniques and the use of thermoplastics. These are plastics that become soft and easy to manipulate when heated (commonly done using hot water). Once heated the plastic is wrapped around the patient's finger to create the splint then left to cool. During the cooling process, however, there is often 'bounce-back', where the plastic distorts slightly due to the change in temperature. The splint therefore doesn't fit the patient accurately, which can affect recovery.
Scope
The aim of this project was to improve the accuracy of finger splints using 3D printing, and explore whether there was an opportunity to create personalised splints based on patient data using associated digital technologies such as a 3D scanner.
Head & Neck Cradle
Initial Problem
Radiology head and neck cradles are used to keep patients' heads still during radiation treatment. In order to maintain an accurate dose of radiation, the patient needs to be fixed in the same position for each treatment. However, the vacuum forming process used to create the cradles produced varied results, therefore making it difficult to provide accurate treatment. Some of the clinical engineers thought 3D printing might act as a more precise form of manufacturing.
Initial Scope
The purpose of using 3D printing was to eliminate inaccuracies that occurred with vacuum forming and manual drilling. This required a full-scale head and neck cradle to be 3D printed at a resolution sufficient enough for proof-of-concept. The print may have to undergo radiation testing, but this would not require or involve a patient.
Rando Simulation Arm
Initial Problem
Initially, the idea was to design and produce arms for Radiology's human simulation model (RANDO) using the mobile 3D scanner to scan my own arm and 3D printing the digital output.
Initial Scope
In order to more accurately test and validate ongoing radiation treatment, the simulation model required arms. The structure of each arm needed to be modeled for the specific simulation model I was working on, and made from a material that attenuates radiation in a similar way to the human body, such as water.
Neonatal Ear Splint
Initial Problem
Ear defects such as 'floppy ear' or 'bat ear', where the top of the ear is folded over or sticks out prominently from the head, are both common birth defects. However, because neonatal ear cartilage is still in early stages of development, these defects can be corrected by fixing the ears in a desired position for 4 - 12 weeks. Existing methods, such as pulling the ear back with adhesive tape or wire, often result in undesirable characteristics - asymmetry and tight folds at the top of the ear. Customised 3D-printed splints may produce a better outcome than what currently exists for correcting neonatal ear defects.
Initial Scope
The initial aim was to design a patient-specific object that applied equal pressure to a neonatal's ear cartilage whilst keeping the ear in a desired position. Due to limitations associated with ethical considerations and the challenges of using baby ear, my own ear was to be used as proof for concept design process.
Acknowledgments
Thanks again to my supervisors Stephen Reay and David White for all of their encouragement and advice during the year, my work colleagues Reid Douglas and Nick Hayes and my brother Luke Munn for their valuable input and the DHW Lab, AUT University and my wife Bridget for ongoing support.
Keywords: 3D printing, design, healthcare, hospital, additive manufacturing, digital technologies, co-design, collaboration, end-users, human-centred design, probes, transparency, CAD, modeling, shared understanding, participatory design, 3D scanning, parametric design.